Immune System Effects
Emerging research suggests that disruptions in the immune system, particularly involving T cells, may play a significant role in the development and persistence of Long COVIDPersistent symptoms following recovery from acute COVID-19. symptoms.
Understanding T Cells and Their Subtypes
T cells are a type of white blood cell crucial for the immune system’s ability to fight infections. They originate from the bone marrow and mature in the thymus, differentiating into various subtypes, including:
- Naive T Cells: These cells have not yet encountered any pathogens. Upon first exposure to a new pathogenA microorganism that can cause disease., naive T cells activate, proliferate, and differentiate into effector cells tailored to combat the specific invader.
- CD4+ T Cells (Helper T Cells): These cells assist other immune cells by releasing cytokines, which enhance the immune responseThe body's defense mechanism against pathogens.. They are pivotal in orchestrating the body’s defense mechanisms.
- CD8+ T Cells (Cytotoxic T Cells): These cells directly attack and destroy infected or malignant cells, playing a critical role in controlling viral infections.1https://pmc.ncbi.nlm.nih.gov/articles/PMC9647062/
Impact of SARS-CoV-2The virus responsible for the COVID-19 pandemic. on T Cells
SARS-CoV-2The virus responsible for the COVID-19 pandemic., the virus responsible for COVID-19A disease caused by the SARS-CoV-2 virus, leading to respiratory illness., has been observed to affect T cells in several ways:
- Reduction in T Cell Counts: Studies have reported a significant decrease in the numbers of CD3+ T cells, including both CD4+ and CD8+ subsets, correlating with disease severity. This lymphopenia suggests an impaired immune responseThe body's defense mechanism against pathogens. in severe cases.2https://pmc.ncbi.nlm.nih.gov/articles/PMC9147674/
- Dysregulation and Activation: In individuals recovering from severe COVID-19A disease caused by the SARS-CoV-2 virus, leading to respiratory illness., there is evidence of prolonged activation of both CD4+ and CD8+ T cells. Elevated levels of activation markers and pro-inflammatory cytokines have been detected up to three months post-infection, indicating sustained immune perturbations.3https://pmc.ncbi.nlm.nih.gov/articles/PMC10319436/
- Alterations in Naive and Memory T Cells: Research indicates a decrease in naive T cell populations and an increase in terminal effector and exhausted T cells, especially among CD8+ subsets. This shift may impair the body’s ability to respond to new infections and contribute to chronic inflammation. 4https://pmc.ncbi.nlm.nih.gov/articles/PMC9226563/
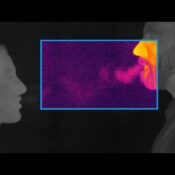
- Potential for Viral Persistence: Some studies suggest that SARS-CoV-2The virus responsible for the COVID-19 pandemic. RNA can persist in certain tissues for extended periods, potentially leading to ongoing T cell activation and contributing to Long COVIDPersistent symptoms following recovery from acute COVID-19. symptoms.5https://pmc.ncbi.nlm.nih.gov/articles/PMC11337933/
Implications for Long COVIDPersistent symptoms following recovery from acute COVID-19.
The observed T cell dysregulation in COVID-19A disease caused by the SARS-CoV-2 virus, leading to respiratory illness. patients may have several implications:
- Impaired Immune Surveillance: A reduction in naive T cells limits the body’s capacity to recognize and respond to other novel pathogens, potentially increasing susceptibility to other infections.
- Chronic Inflammation: Persistent activation of T cells can lead to ongoing inflammation, which is associated with many Long COVIDPersistent symptoms following recovery from acute COVID-19. symptoms, such as fatigue and cognitive difficulties.
- Autoimmunity Risk: Dysregulated T cell responses may increase the risk of developing autoimmune conditions, where the immune system mistakenly attacks the body’s own tissues.
Conclusion
The interplay between SARS-CoV-2The virus responsible for the COVID-19 pandemic. and the immune system, particularly T cells, is complex and still under investigation. Understanding how this virus affects T cell function and regulation is crucial for developing targeted therapies and management strategies for Long COVIDPersistent symptoms following recovery from acute COVID-19.. Ongoing research aims to elucidate these mechanisms to improve patient outcomes.